August 18, 2025
Understanding the Link Between Allergies and Asthma: What You Need to Know

Allergies and asthma are two conditions that affect millions of people, and while they may seem unrelated, they’re often closely connected. For many, the same substances that cause sneezing, itchy eyes, or a runny nose can also trigger asthma symptoms like wheezing or shortness of breath. When asthma is triggered by allergens, it is called allergic asthma. This overlap—known as allergic asthma—can make life more challenging if you don’t address both conditions together.
At Greater Austin Allergy, we see this connection every day. Our providers help patients identify their triggers, manage symptoms, and create treatment plans that address both allergies and asthma for lasting relief. Managing both your allergies and asthma together is essential for optimal results.
Introduction to Asthma
Asthma is a chronic respiratory disease that affects the airways in your lungs, making it harder to breathe when symptoms flare up. At its core, asthma is caused by inflammation and bronchospasm—meaning the lining of your airways swells and the muscles around them tighten. This combination can lead to classic asthma symptoms like coughing, wheezing, chest tightness, and shortness of breath. When these symptoms become severe, it’s known as an asthma attack, which can be a medical emergency.
For many people, asthma is closely linked to the immune system’s response to common allergens. If you have allergic diseases, your immune system may overreact to harmless substances like pollen, dust mites, or pet dander, causing an allergic reaction. In some cases, this allergic response doesn’t just cause sneezing or a runny nose—it can also trigger inflammation and mucus buildup in your airways, leading to what’s called allergy induced asthma or allergic asthma. Understanding how your immune system reacts to these common allergens is key to managing both your allergy and asthma symptoms effectively.
How Allergies and Asthma Are Connected
Allergic asthma occurs when allergens—like pollen, dust mites, mold spores, pet dander, animal dander (a common year-round allergen that can trigger asthma symptoms), or even cockroach droppings—trigger asthma symptoms. Here’s what’s happening in your body:
- With allergies, your immune system mistakes a harmless substance for a dangerous one and overreacts.
- With asthma, your airways become inflamed and narrow, making it harder to breathe.
- When they combine, exposure to an allergen can set off a chain reaction: your immune system responds, inflammation increases, mucus builds up, and airways tighten—leading to an asthma flare-up.
Allergic rhinitis, also known as hay fever, often coexists with asthma and can cause symptoms like nasal congestion and sneezing.
People with a family history of allergies, asthma, hay fever, or allergic rhinitis are more likely to develop both, and symptoms can start at any age.
Recognizing the Overlap
Allergy symptoms often include sneezing, a runny or stuffy nose, itchy or watery eyes, and skin reactions.
Asthma symptoms include coughing, wheezing, chest tightness, and shortness of breath.
When you have both allergies and asthma, the symptoms can blend together, making it harder to tell which condition is acting up—and sometimes, both are. You may start to notice patterns, such as:
- Your asthma symptoms flaring during high pollen seasons, especially when tree pollen is present, even if your usual asthma control plan was working fine before.
- Indoor triggers like pet dander, dust mites, or mold causing both nasal congestion and difficulty breathing.
- Food allergies can also trigger both allergy and asthma symptoms in some individuals.
- Allergy-related inflammation making your airways more sensitive, so even mild triggers set off coughing or wheezing.
- A frustrating cycle where treating one condition provides some relief but never fully resolves your symptoms because the other condition is still active.
At Greater Austin Allergy, we can help break this cycle by identifying your specific triggers and creating a coordinated plan to manage both conditions together, so you’re not left chasing symptoms.
Common Allergens
When it comes to allergic asthma, certain allergens are the usual suspects behind flare-ups and uncomfortable symptoms. Dust mites are tiny creatures that thrive in bedding, upholstery, and carpets, feeding on skin flakes and thriving in warm, humid environments. Mold spores, often found in damp areas like bathrooms or basements, can become airborne and easily trigger asthma symptoms when inhaled. Pet dander—tiny flakes of skin and hair from cats, dogs, and other furry animals—can linger in the air and on surfaces, causing allergic reactions in sensitive individuals. Pollen from trees, grasses, and weeds is a major culprit during allergy season, often making asthma symptoms worse for those with seasonal allergies. Even cockroach droppings, which contain potent proteins, are a common allergen in many homes, especially in urban areas.
Recognizing these common allergens and understanding how they can trigger allergic asthma is the first step toward reducing your exposure and keeping your asthma symptoms under control. By identifying your specific triggers, you can take targeted steps to prevent allergic reactions and avoid asthma attacks.
How Allergies Can Trigger Asthma Attacks
When allergens enter your body—whether through your nose, mouth, or even your skin—your immune system can overreact. This overreaction causes inflammation in the nasal passages and airways. As the inflammation builds, your body produces more mucus, and the muscles around your airways tighten, making it harder to breathe. This tightening can result in an allergic asthma attack, which may be more severe than typical asthma attacks.
These reactions can happen in two ways:
- Immediate response: Symptoms appear within minutes of exposure to an allergen. You may start coughing, wheezing, or feeling chest tightness soon after contact.
- Delayed response: Symptoms develop over several hours as inflammation continues to build, which can lead to a second wave of breathing difficulties.
Common asthma triggers such as secondhand smoke, dust mites, and air pollution can provoke or worsen these reactions.
Certain factors can make these reactions even worse:
- Environmental conditions like high humidity, sudden temperature changes, or exposure to cold air.
- Airborne irritants such as smoke, secondhand smoke, strong fragrances, or air pollution.
- Multiple triggers at once—for example, being exposed to pollen on a day when the air quality is poor.
Other triggers, such as strong emotions or exercise, can also provoke asthma symptoms.
The more your airways are exposed to allergens, the more sensitive they can become over time, which means even small amounts of exposure can set off symptoms.
Why Integrated Management Matters
Treating just your allergies or just your asthma is like fixing half a problem—you might get some relief, but symptoms will keep coming back.
Here’s why an integrated approach works best:
- Uncontrolled allergies can keep your asthma flaring.
- Poorly managed asthma can make allergy symptoms harder to control.
- Not managing both allergies and asthma together can lead to uncontrolled asthma, increasing the risk of severe symptoms and complications.
At Greater Austin Allergy, our providers can coordinate both allergy and asthma care under one roof—combining medication, immunotherapy, and trigger avoidance strategies for better long-term control. For those with severe allergic asthma, advanced treatments and close monitoring may be necessary to effectively manage the condition.
Practical Management and Prevention Tips
Managing allergies and asthma together doesn’t have to feel overwhelming—it’s about making small, consistent changes that add up to fewer flare-ups and better breathing. Here are some real-world strategies our team at Greater Austin Allergy often recommends: Avoiding triggers is crucial to prevent attacks, so identifying and minimizing exposure to allergens like dust mites, pet dander, and mold can make a significant difference.
At Home
Think of your home as your “safe zone” from triggers.
- Clean smarter, not harder: Use a vacuum with a HEPA filter and dust with a damp cloth so you’re trapping allergens, not spreading them around.
- Wash it away: Change bedding weekly in hot water to fight dust mites and consider dust-mite-proof covers for pillows and mattresses.
- Breathe clean air: An air purifier with a HEPA filter in your bedroom can make a big difference, especially at night when you’re sleeping and your body is repairing itself.
- Watch humidity: Keep it between 30–50% to prevent mold growth.
In addition to these steps, a medicine called biologic may help manage allergic asthma symptoms at home by targeting the underlying allergic response.
During Allergy Season
When pollen counts are high, a few smart swaps can help keep symptoms in check.
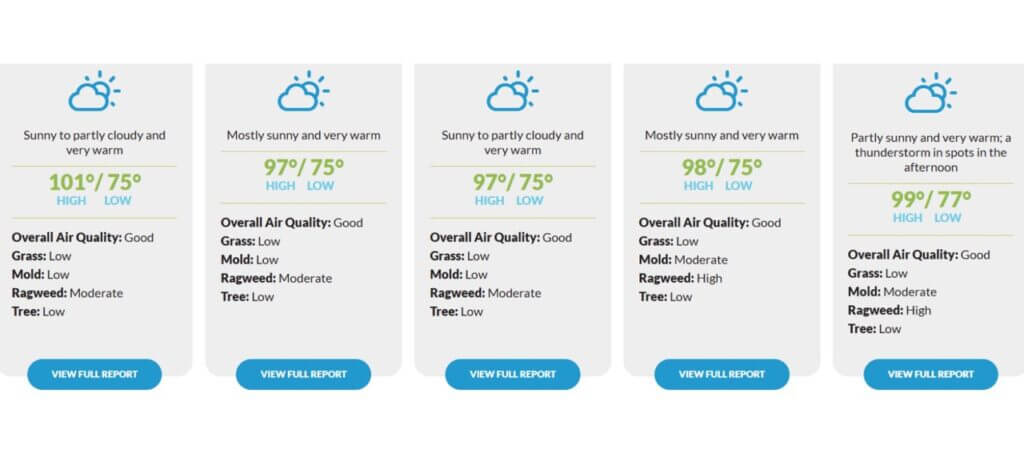
- Check before you step out: Use ourLocal Allergy Report so you know what’s in the air that day.
- Change and shower: After being outdoors, swap into clean clothes and shower to remove pollen from your skin and hair.
- Plan your outings: Try to run errands or exercise outdoors early in the morning or later in the evening when pollen levels are lower.
Medications
A tailored treatment plan can be the difference between “barely getting through the day” and actually enjoying it.
- Asthma inhalers keep your breathing steady—quick relief inhaler for sudden symptoms, long-term control for prevention.
- Allergy medications like antihistamines, nasal sprays, or leukotriene modifiers can calm your body’s overreaction to allergens.
- Preventive care might include daily inhaled corticosteroids or allergy shots/drops, a treatment called immunotherapy, to reduce your sensitivity over time.
Long-Term Solutions
If you want to stop playing defense and start taking control, long-term solutions are key.
- Allergy testing helps pinpoint your exact triggers, so you’re not guessing.
- Immunotherapy works like training for your immune system—gradually reducing its overreaction so you can live with fewer symptoms year after year.
The best plan is one that’s built around your lifestyle, your triggers, and your goals—and that’s exactly what we do at Greater Austin Allergy.

Asthma Action Plan
An Asthma Action Plan is a personalized, step-by-step guide designed to help you manage your asthma symptoms and prevent asthma attacks before they start. Created in partnership with your healthcare provider, this plan outlines exactly what to do when you notice changes in your symptoms, how to use your medications correctly, and which triggers to avoid. It also provides clear instructions on when to seek medical help and how to adjust your treatment if your asthma gets worse.
Having an asthma action plan empowers you to take control of your asthma, helping you prevent asthma attacks and keep your symptoms in check. It’s important to review your plan regularly with your healthcare provider to make sure it stays up to date with your current needs and treatment options. With a well-crafted asthma action plan, you can feel more confident in managing your asthma and living life on your terms.
Climate Change and Asthma
Climate change is having a growing impact on people with asthma, making symptoms more frequent and severe for many. Rising temperatures and shifting weather patterns can lead to longer allergy seasons and higher pollen counts, which can trigger asthma symptoms and increase the risk of asthma attacks. Increased air pollution, more frequent wildfires, and changes in humidity can also make it harder for people with asthma to breathe easily.
For those with allergic asthma, these environmental changes mean more exposure to airborne allergens and potential triggers. Staying informed about local air quality, pollen forecasts, and weather conditions can help you anticipate and avoid situations that might make your asthma worse. As climate change continues to affect our environment, proactive asthma management and awareness of potential triggers are more important than ever for keeping your symptoms under control.
When to Seek Medical Help
Call Greater Austin Allergy if:
- Your asthma symptoms are getting worse or aren’t controlled by your current plan.
- Allergy symptoms aren’t improving with over-the-counter or prescribed medications.
Seek emergency care if you have:
- Severe asthma attacks.
- Difficulty speaking due to shortness of breath.
- Bluish lips or fingernails.
- Rapid breathing or chest retractions.
Better Breathing Begins Here
Allergies and asthma may share a frustrating connection, but that doesn’t mean they have to run your life. Once you understand how one can trigger the other, you can start making choices that keep both in check—whether that’s avoiding certain triggers, staying ahead of allergy season, or finding the right mix of treatments.
At Greater Austin Allergy, we believe no one should settle for “just getting by.” Our team works with you to uncover your unique triggers, create a plan that tackles both conditions, and give you the tools to breathe easier—on your best days and your worst.
If your allergies are making your asthma harder to control, let’s change that. Schedule an appointment with us and take the first step toward better breathing and a healthier you.
